Populism and Corrupt Courts
Thank you to my wonderful friend Carolyn Conrad for saving many of the posts I wrote for the now-defunct Examiner.com.
Carolyn’s son Christopher died recently. He never fully recovered from the devastation thrust upon his life by corrupt court collaterals and judicial officers. Ah, that tears could wash away the memories. But not.
UAMS Doctors Tried to Hide the Evidence
Summary of the Case
This complaint arises from negligence in a medical setting that can be understood by a person of ordinary intelligence using common knowledge. The defendants failed to ask the patient what the mechanism of his injury was, instead relying on an unattributed and erroneous note made by someone who was not a witness to the accident. Based solely on that erroneous statement, the Medical Defendants substituted their judgment for the patient’s and refused to allow the patient to contact his family or get a ride home from a professional driver.
The claims that arose during the two weeks immediately after are brought under two alternate theories. The Plaintiffs’ preferred theory is that refusal of consent ended the doctor-patient relationship, and the further claims arise out of ordinary tort, contract, and civil rights law. The alternative is that Lynn’s claims are subsumed into the medical injury claim, and Hammett’s claims fall under tort, contract, and civil rights law, particularly the ADA.
In response to the Plaintiffs’ threats of a lawsuit, the Defendants allowed Lynn to leave the hospital on January 27, 2024. Instead of attempting to make the Plaintiffs whole, the Defendants manifested their intent to commit fraud on the court and obstruct justice. They refused to amend the medical record to correct the mechanism of the initial injury and destroyed the videos taken in the emergency room and during Lynn’s escape attempts through the hospital halls and stairways.
ABC Guide to Lawyering

This book was actually my son Sean’s idea, and it’s published through his Amazon account. Amazon takes the bulk of the sale price—Sean says he earns only a few cents per copy—but his goal was never the money. He wants to share what he went through: the medical battery and false imprisonment he endured at UAMS, and the obstacles he’s faced while pursuing a settlement with the state-run hospital.~~~
There is a lengthy sample that you can read on your phone. It is a good long-weekend-cozy-in-bed book.
Another Toothless Tiger Law
This would be a wonderful law, except that recovery under the law relies on government prosecution of corrupt judicial officers. In other words, it will almost never happen.
A.C.A. § 16-106-111
§ 16-106-111. Exception to judicial immunity
(a) The General Assembly finds that:
(1) The common law doctrine of judicial immunity from civil suit has been accepted by the courts under Peterson v. Judges of Jefferson County Circuit Court, 2014 Ark. 228 (per curiam) and Pierson v. Ray, 386 U.S. 547 (1967), and is state law; and
(2) An exception to this blanket grant of judicial immunity is necessary to protect the public from certain criminal and unethical acts committed by judges and justices.
(b) A person who has had an adverse decision against him or her in a court in this state may file a claim in the circuit court with jurisdiction against a judge or justice who made the adverse decision in the judge or justice’s individual capacity if the judge or justice:
(1) Made or influenced the adverse decision as a result of bribery;
(2) Has been found guilty of, or pleaded guilty to, nolo contendere to, or the equivalent of nolo contendere to, a criminal offense for conduct constituting bribery in any state or federal court; and
(3) The bribery conviction described in subdivision (b)(2) of this section resulted from the conduct described in subdivision (b)(1) of this section.
(c) A person is entitled to the following remedies if he or she prevails on a claim under subsection (b) of this section:
(2) Damages, including without limitation punitive damages; and
(d) A prosecuting attorney may bring a cause of action under this section, and may, in his or her discretion, use any proceeds recovered in the proceeding to:
(1) Cover the prosecuting attorney’s costs of the proceeding in which the adverse decision described in subsection (b) of this section occurred;
(2) Give to the victim or the estate of the victim of the crime that the prosecuting attorney was prosecuting in the proceeding in which the adverse decision described in subsection (b) under this section occurred;
(3) Donate to a nonprofit victims’ rights advocacy group; or
(4) Donate to the State Treasury.
(e) The statute of limitations for a cause of action under this section:
(2) Begins to run the day the judge or justice is found guilty of, or pleads guilty to, nolo contendere to, or the equivalent of nolo contendere to, a criminal offense for conduct constituting bribery in any state or federal court.
(f)(1) If a cause of action is timely filed under this section and the judge or justice is deceased at the time of the filing or dies during the pendency of the cause of action, the person or the estate of the person filing the cause of action may proceed against the estate of the judge or justice.
(2) The estate of a person may proceed with a cause of action under this section against a judge, justice, or the estate of the judge or justice, if the person dies before the cause of action accrues or during the pendency of the action.
(1) “Adverse decision” means a ruling in which a judge’s or justice’s order differs from the relief or request sought by a litigant on a motion or objection in a civil or criminal matter;
(2) “Bribery” means giving, offering, accepting, or agreeing to accept money or any other benefit, pecuniary or otherwise, for the purpose of affecting the outcome of a court proceeding or decision; and
(3) “Person” means any individual, corporation, business trust, estate, trust, partnership, limited liability company, association, joint venture, government, governmental subdivision, agency, or instrumentality, public corporation, or any other legal or commercial entity.
UAMS Torture Victim in His Own Words
Arkansas Claims Commissioners Dee Holcomb, Henry Kinslow, and Paul Morris issued a sua sponte order on November 14, 2025, denying ADA accommodations to a disabled man. Sean Lynn is suing UAMS for imprisoning and battering him for two weeks in 2024. The torture resulted in a disrupted oscillator chain in his left ear and exacerbated aphasia that lingers on two years later.
Being drugged with Fentanyl, a list of benzodiazepines, and barbiturates, then bound to a bed, naked for much of the time, and chased down hallways and stairs when trying to escape, caused Lynn symptoms of PTSD.
Holcomb, Kinslow, and Morris said that when I, a co-claimant and Sean’s mother, wrote our joint documents, I was engaged in the unauthorized practice of law. The Commissioners made a vague reference to some unnamed persons who may or may not have been co-claimants and may or may not have had communication disabilities, who were not allowed to join on documents they filed.
The Commissioners wrote: “While Ms. Hammett is entitled to represent herself before the Commission with regard to her individual claims, any attempt by her to represent Mr. Lynn would appear to be the unauthorized practice of law (and similar attempts have been rejected in other matters).”
The Commissioners might claim that they did not say I attempted to represent Mr. Lynn, as “any” could mean there was no attempt, but if there was an attempt, it would “appear” to be criminal conduct. The last corrupt jurist I dealt with, Federal Judge Lee P. Rudofsky, disagreed with that interpretation of the word “any.” When I wrote that “any” credit card usage I made on a Capital One Account was for consumer goods, and therefore subject to the FDCPA, Judge Rudofsky said that was an admission that I used the credit card and did not pay it off. The Eighth Circuit Court of Appeals agreed with Judge Rudofsky wholeheartedly.
I think the language of the order issued by the Commissioners gives them the wiggle room to say they were expressing “concern” and not making a definitive statement. But if Sean and I did not object and ask for reconsideration of the order, history would be rewritten, and the law of the case and issue preclusion would say that I was practicing law without a license.
Inexplicably, the Commissioners have looked at our claims for over a year and never expressed one bit of concern that doctors and nurses at UAMS forced Sean to ingest dangerous drugs, used physical restraints, and catheterized him instead of letting him get up to use the toilet over a two-week period– without offering him an attorney to defend him from this false imprisonment. UAMS PD refused to investigate our allegations of criminal conduct by UAMS staff. And UAMS Security deleted all the videos of the alleged criminal conduct.
The YouTube video of one of the many discussions Sean and I had about the torture at UAMS was posted three days ago, but it was recorded about a year ago. It is on Sean’s YouTube channel. Show your support for autonomy over our bodies and access to justice by liking and subscribing.
Arkansas Claims Commission Questions Whether Claimant Is Entitled to ADA Accommodations; Shows No Concern that UAMS Doctors Falsely Imprison and Batter “Patients”
Arkansas Claims Commissioners Dee Holcomb, Henry Kinslow, and Paul Morris issued an order today in the civil claim that alleges doctors and other medical staff at UAMS committed criminal battery and false imprisonment against a man who hit his head when he jumped from the 10-foot-high rung of a falling ladder. Aphasia caused by a stable brain bleed was exacerbated by forced drugging and smashing the patient’s head against hard objects to physically restrain him in the $10,000 per night hospital room. The Commissioners expressed concern that the patient’s co-claimant and accommodator was practicing law. The Commissioners did not express any concern whatsoever about the battery, false imprisonment, and destruction of evidence by the half-million-dollar-per-year salaried doctors at the state-run hospital.
Here are the order and a motion for reconsideration that were both filed today.
UAMS Attorney and Insurer Playing Stupid Tricks

The two envelopes above supposedly delivered the same documents to two claimants. Ooops! Look at the metered postage.
The reason UAMS attorneys and insurance agents wanted to withhold the actual documents from me, one of the joint claimants on a case stemming from false imprisonment and battery, is that they caused partial deafness, aphasia, and PTSD in the other claimant. Now they don’t want him to have ADA accommodations during the proceedings.
I am incredibly busy, between my 1L year in law school and trying to make the state-run hospital pay restitution. So, I am going to just post our latest documents below. Enjoy the read.





Does UAMS Attorney Hallucinate; Or Does She Use ChatGPT? [Redacted for error on 11/1/2025]
My sincere apology. It is I who made the error, quoting the Federal Rules of Civil Procedure, instead of the Arkansas rules, which do use the word “amend.”
Still, UAMS chose to lie to the Commission by submitting the original answers. UAMS’s counsel has access to the authors of the medical record and is paid to read the record; yet, counsel failed to admit that there was no written consent by Lynn to be found when she wrote the original responses.
You can download the full documents that were filed in this volley of motion practice, here:
Judge Susan Weaver Authorized Prejudgment Taking of Real Estate
Orders issued by Judge Susan Weaver in Arkansas that transferred 40 acres and a house were challenged to the Arkansas Court of Appeals. The appellee failed to file an opposition.
A year later, the COA issued an order denying the appeal, based on what the court said was a lack of jurisdiction. The Court of Appeals judges said the case was not final when the appeal was filed.
But, the property had already been transferred!
Here is a quote from my 1L Civil Procedure textbook, quoting a U.S. Supreme Court case from 1991.
“This case requires us to determine whether a state statute that authorizes prejudgment attachment of real estate without prior notice or hearing, without a showing of extraordinary circumstances, and without a requirement that the person seeking the attachment post a bond, satisfies the Due Process Clause of the Fourteenth Amendment. We hold that, as applied to this case, it does not.” Connecticut v. Doehr, 501 U.S. 1 (1991).
An attachment does not necessarily dispose of property. The transfer of title Judge Weaver made allowed the Plaintiff to transfer the property to an irrevocable trust, who sold it to a third party, a sheriff. There was no bond required in Pietrczak v. Rural Revival Living Trust and Laura Lynn, 65CV-21-20. In fact, Laura Lynn (this blogger) was already dismissed with prejudice as a Common-Defense-Doctrine defendant. The trust was in default because there was no attorney willing to fight against Judge Weaver, who obviously favored the plaintiff’s attorney, William Zac White.
Before Mr. White got involved, Pietrczak was represented by Billy Jack Gibson, who became a judge. There is a fun little tidbit at the end of the post about the Gibson-Pietrczak connection that you won’t want to miss.
There were no extraordinary circumstances shown on the record, as to why the property should be attached before a final judgment issued. The property was in escrow within a couple days and the purchaser asked a neighbor what happened to the personal property that was in the house when they saw it…clearly before the order to transfer to Pietrczak was signed. That was a bit extraordinary. Judge Susan Weaver might have the superpower of ESP.
The most troubling part is that the appellate judges in Arkansas opined sua sponte that they had no jurisdiction, but did not notice that an old lady’s property was seized without due process. Remember the names: Judge Rita Gruber. Judge Cindy Thyer. Judge Brandon Harrison.
Now the juicy gossip. Mike Pietrczak had charges filed against him in January 2025 for assault in the 3rd degree, resisting arrest, and failure to appear. MVC-25-45. The warrant was finally served on September 18, 2025. Then on September 22, 2025, a citation was filed against Micheal (correct spelling) Pietrczak for criminal mischief in the 2nd degree, disorderly conduct, and public intoxication in the 1st degree. MVC-25-441. Who is the judge on both cases? Billy Jack Gibson.
For some reason, Judge Gibson doesn’t recuse himself from presiding over criminal cases against a past client whom Mr. Gibson helped to defraud me of my property.
By the time I find an honest judge to reverse the legalized thievery of my assets, Pietrczak will have drank the money or paid it all to the lawyer types who give him a get out of jail free card.
UAMS Attorney Sherri Robinson Lies Again.
The Senior Associate General Counsel at UAMS certified the following statement in answer to a third amended claim for medical injury, perjury, and breach of fiduciary duty by the doctors, residents, security, and administrators at UAMS.
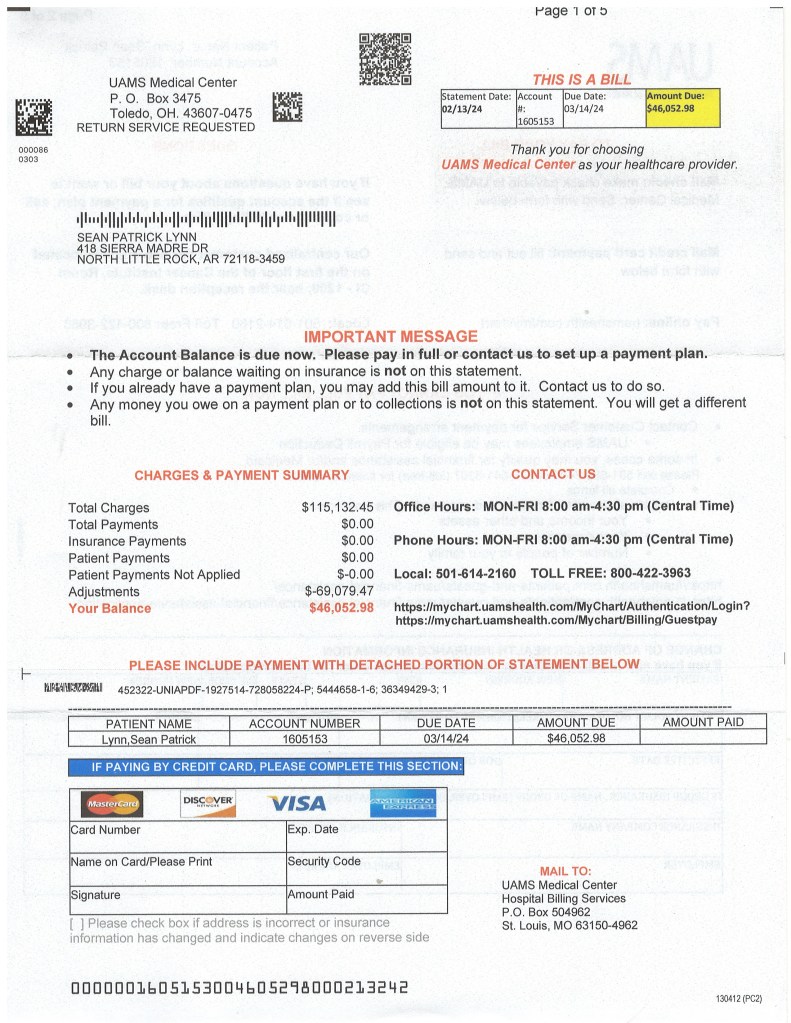
“With regard to paragraph 67, UAMS admits that two documents entitled ‘Billing Detail by Date’ were sent to Lynn on February 21, 2025, with one setting forth a balance of $42,09.78 and the other a
balance of $4,188.40. UAMS denies that the documents ‘demanded payment,’ and affirmatively plead that both documents contained the following statement: This is not a bill. The font color and underlining
were present in the original documents sent to Lynn as well.” (“This is not a bill” was underlined and in red in the answer.)
Paragraph 67 asserts in full: “UAMS sent a bill to Lynn, upon his release, demanding $42,095.78 plus a
separate bill demanding an additional $4,188.40 for a total of $46,284.18.”
There was no reference made to the “not a bill”. A copy of the bill, produced to UAMS at the same time as the “not a bill”, is posted above.
This seems like good evidence to corroborate our claim that UAMS committed fraud. It is their pattern of practice.
Mrs. Robinson may try to claim that she didn’t actually lie. She did not deny that UAMS sent the bill for $46,284.18. She only denied that the other documents, the ones titled “Billing Detail by Date,” were a bill.
What do you think? Was this lack of candor to a tribunal a “lie”? A fib? Or a perfectly acceptable answer in response to the assertion that UAMS sent a bill for over forty-six thousand dollars to a man who pleaded to be released from imprisonment for two weeks.
The claim and answer are available to download below.
As a personal aside, my husband was diagnosed with stage four prostate cancer metastasized to everywhere last November. His PCP referred him to UAMS. He refused to go to UAMS and went instead to Carti. Carti did a fabulous job, and my husband’s PSA went from 1,299 to well under 1. I’m pretty sure if he went to UAMS, he would be dead, and UAMS would bill a half a million dollars for their treatment.
P.S. Notice that the bills are generated and sent from Ohio. Payments are mailed to and processed in Missouri. Why is the University of Arkansas sending jobs out of state? The lead attorney on this case is paid over $160,000 per year. Several of the doctor-professors are paid over half a million dollars per year. And, presuming the out-of-state vendors are cheaper than Arkansas companies, UAMS cuts corners when it comes to the common person’s job generation.